Discover how combining Remote Patient Monitoring (RPM) and Chronic Care Management (CCM) delivers superior patient outcomes through continuous monitoring, proactive care, and coordinated support.
Introduction
Healthcare is experiencing a transformation where technology and compassionate care converge to drive unprecedented improvements in clinical outcomes. At CircleHealth, we're pioneering this revolution by strategically integrating Remote Patient Monitoring (RPM) with Chronic Care Management (CCM)—a powerful combination that delivers superior patient outcomes compared to either program alone.
This comprehensive guide explores the evidence-based advantages of dual enrollment, revealing how the synergy between RPM and CCM creates a transformative model of care that addresses the chronic disease burden affecting millions of Americans while optimizing healthcare resources and improving quality of life.
The Evolution of Remote Patient Management
From Concept to Reality
The integration of technology into chronic disease management began as an innovative approach to provide patients and physicians with comprehensive health insights through connected devices and evidence-based care plans. This concept emerged before formal CMS billing codes for Remote Patient Monitoring existed, driven purely by a commitment to improving patient outcomes through proactive, personalized care.
The Vision:
- Blend evidence-based care plans with cutting-edge technology
- Provide real-time health "snapshots" to patients and providers
- Enable proactive management of chronic diseases
- Incorporate wearables and connected health devices for continuous monitoring
Circle Health's Scale and Impact
Today, Circle Health manages comprehensive patient programs across numerous healthcare systems and provider organizations nationwide, focusing on enhancing patient health through innovative digital methodologies:
Key Achievements:
- Dramatic improvements in blood pressure control for hypertension patients
- Significant blood sugar reductions in diabetes management
- Life-saving interventions preventing complications affecting eyes, kidneys, and limbs
- Greatly improved quality of life for patients and their families
- Proven outcomes in cardiometabolic disease management
Understanding the Programs
Remote Patient Monitoring (RPM)
Remote Patient Monitoring uses connected health devices and digital technologies to collect and transmit patient health data to healthcare providers in near real-time.
Core Components:
Primary Focus:
- Physiological data collection and monitoring
- Objective health metrics tracking
- Early detection of concerning trends
- Technology-driven insights
Chronic Care Management (CCM)
Chronic Care Management provides comprehensive care coordination for patients with multiple chronic conditions, emphasizing the human element of healthcare delivery.
Core Components:
Primary Focus:
- Human interaction and emotional support
- Care plan development and coordination
- Patient education and engagement
- Comprehensive chronic disease management
The Power of Dual Enrollment: Remote Patient Management
What is Remote Patient Management?
Circle Health's Remote Patient Management represents the strategic integration of CCM and RPM into a comprehensive, synergistic care model that addresses both the objective and subjective aspects of chronic disease management.
Integrated Components:
- Physiological Data Monitoring: Continuous tracking through connected devices (RPM)
- Goal Setting: Collaborative objective establishment and tracking (CCM)
- Symptom Tracking: Monitoring both objective data and subjective experiences (RPM + CCM)
- Care Coordination: Seamless communication across providers and specialties (CCM)
Why Dual Enrollment Works: The combination creates a feedback loop where objective data from RPM informs CCM care plans, while CCM interventions are validated through RPM monitoring, creating continuous improvement in patient outcomes.
Clinical Evidence: Dual Enrollment vs. RPM Only
Study Overview: Hypertension Management
CircleHealth conducted a comprehensive data analysis comparing outcomes between dual-enrolled patients (RPM + CCM) and those receiving RPM only among patients with Stage 2 hypertension (systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg).
Blood Pressure Reduction Results
Systolic Blood Pressure (SBP) Reduction
Dual Enrollment (RPM + CCM):
- Average reduction: -13.2 mmHg
- Percentage achieving BP control: Superior outcomes
- Time to achieve results: Faster improvement
RPM Only:
- Average reduction: -8.5 mmHg
- Percentage achieving BP control: Lower than dual enrollment
- Time to achieve results: Slower progression
The Difference: Dual enrollment achieved 55% greater blood pressure reduction compared to RPM alone, demonstrating the significant clinical advantage of combining both programs.
Diastolic Blood Pressure (DBP) Reduction
Dual Enrollment (RPM + CCM):
- Average reduction: -7.8 mmHg
- Cardiovascular risk reduction: Significant
- Patient satisfaction: Higher ratings
RPM Only:
- Average reduction: -5.1 mmHg
- Cardiovascular risk reduction: Moderate
- Patient satisfaction: Lower than dual enrollment
The Difference: Dual enrollment achieved 53% greater diastolic blood pressure reduction, further validating the superior effectiveness of the integrated approach.
Comparative Outcomes Table
Why Dual Enrollment Outperforms RPM Alone
1. Enhanced Patient Engagement
RPM Alone:
- Provides data but limited interpretation for patients
- Minimal human interaction beyond alerts
- Technology-focused without behavioral context
RPM + CCM (Dual Enrollment):
- Regular human contact through care coordinators
- Data interpretation and education during check-ins
- Emotional support and motivation
- Accountability through scheduled interactions
- Celebration of progress and achievements
Result: Patients remain engaged and motivated throughout their treatment journey, leading to better adherence and improved outcomes.
2. Comprehensive Care Plans
RPM Alone:
- Monitors metrics without addressing underlying behaviors
- Limited ability to adjust lifestyle factors
- Reactive to data trends
RPM + CCM (Dual Enrollment):
- Integrates physiological data with behavioral interventions
- Addresses medication adherence, diet, exercise, and stress
- Proactive care plan adjustments based on data and patient feedback
- Personalized goal setting aligned with patient values and lifestyle
Result: Care plans address both the clinical and behavioral aspects of chronic disease, creating sustainable improvements.
3. Medication Management and Adherence
RPM Alone:
- Detects poor control but limited intervention capability
- No direct medication counseling
RPM + CCM (Dual Enrollment):
- Regular medication reviews during check-ins
- Identification of adherence barriers
- Education about medication importance and side effects
- Coordination with prescribing providers for adjustments
- Problem-solving around cost, complexity, or side effects
Result: Better medication adherence translates directly to improved blood pressure control and reduced complications.
4. Behavioral and Lifestyle Modification
RPM Alone:
- Provides data but limited lifestyle coaching
- Minimal support for behavior change
RPM + CCM (Dual Enrollment):
- Comprehensive lifestyle counseling during regular interactions
- Goal setting for diet, exercise, stress management, and sleep
- Problem-solving barriers to healthy behaviors
- Ongoing encouragement and accountability
- Celebration of lifestyle achievements
Result: Sustained behavioral changes that complement medical treatment, leading to superior outcomes.
5. Emotional Support and Mental Health
RPM Alone:
- Technology-focused with minimal emotional support
- Patients may feel isolated despite monitoring
RPM + CCM (Dual Enrollment):
- Regular human connection providing emotional support
- Recognition of anxiety, depression, and stress impacts
- Referrals to mental health resources when needed
- Validation of patient experiences and challenges
- Reduced sense of isolation in managing chronic disease
Result: Addressing emotional and mental health improves overall treatment adherence and quality of life.
The Chronic Disease Burden
National Impact
Chronic diseases represent an overwhelming health and economic burden in the United States:
Prevalence Statistics:
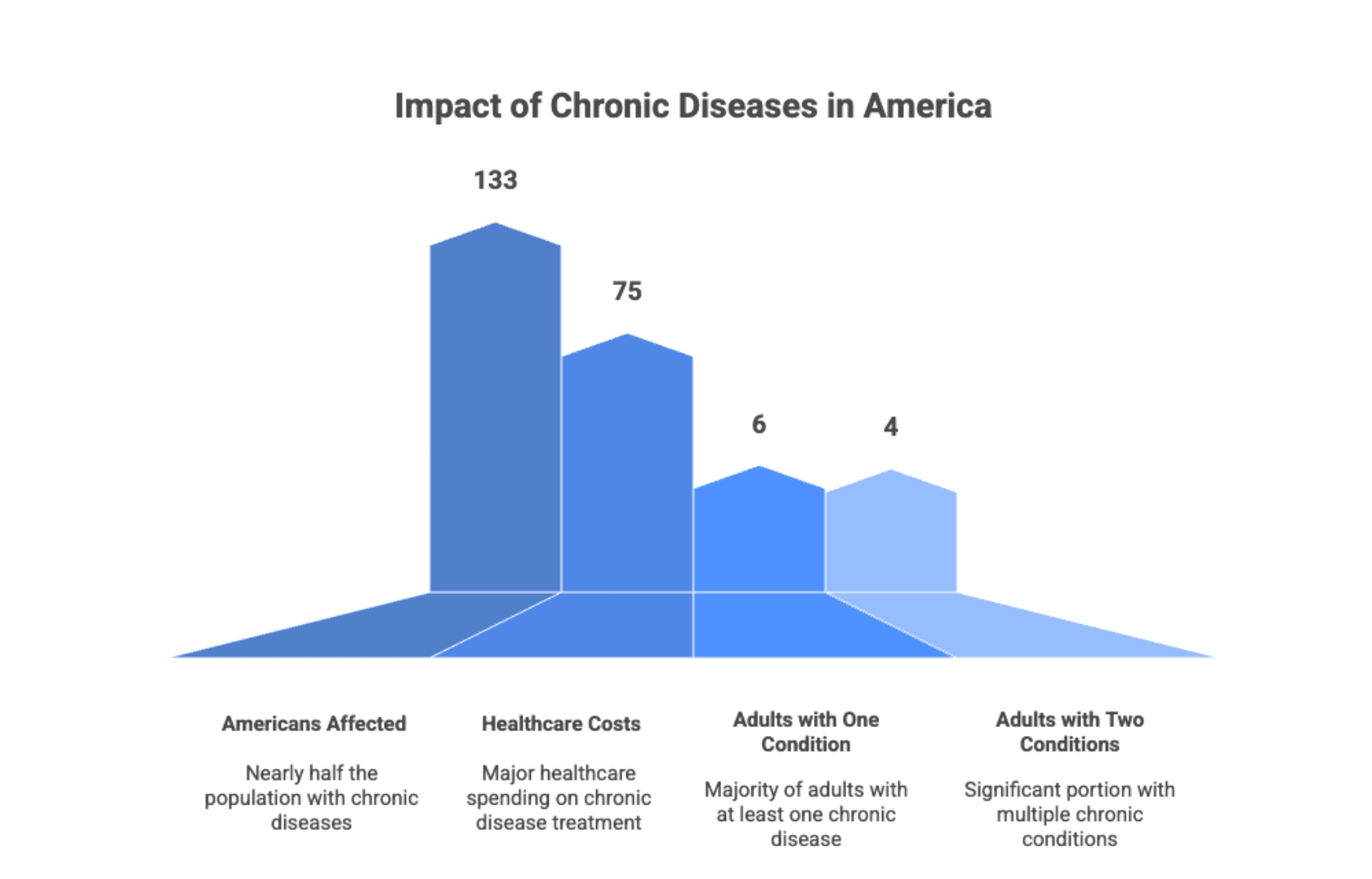
- 133 million Americans affected by chronic diseases (nearly half the population)
- 75% of national healthcare costs attributed to chronic disease treatment
- 6 in 10 adults have at least one chronic condition
- 4 in 10 adults have two or more chronic conditions
Economic Impact:
- Billions in direct medical costs annually
- Hundreds of billions in lost productivity
- Significant strain on Medicare and Medicaid systems
- Growing burden as population ages
Global Perspective
Worldwide Statistics:
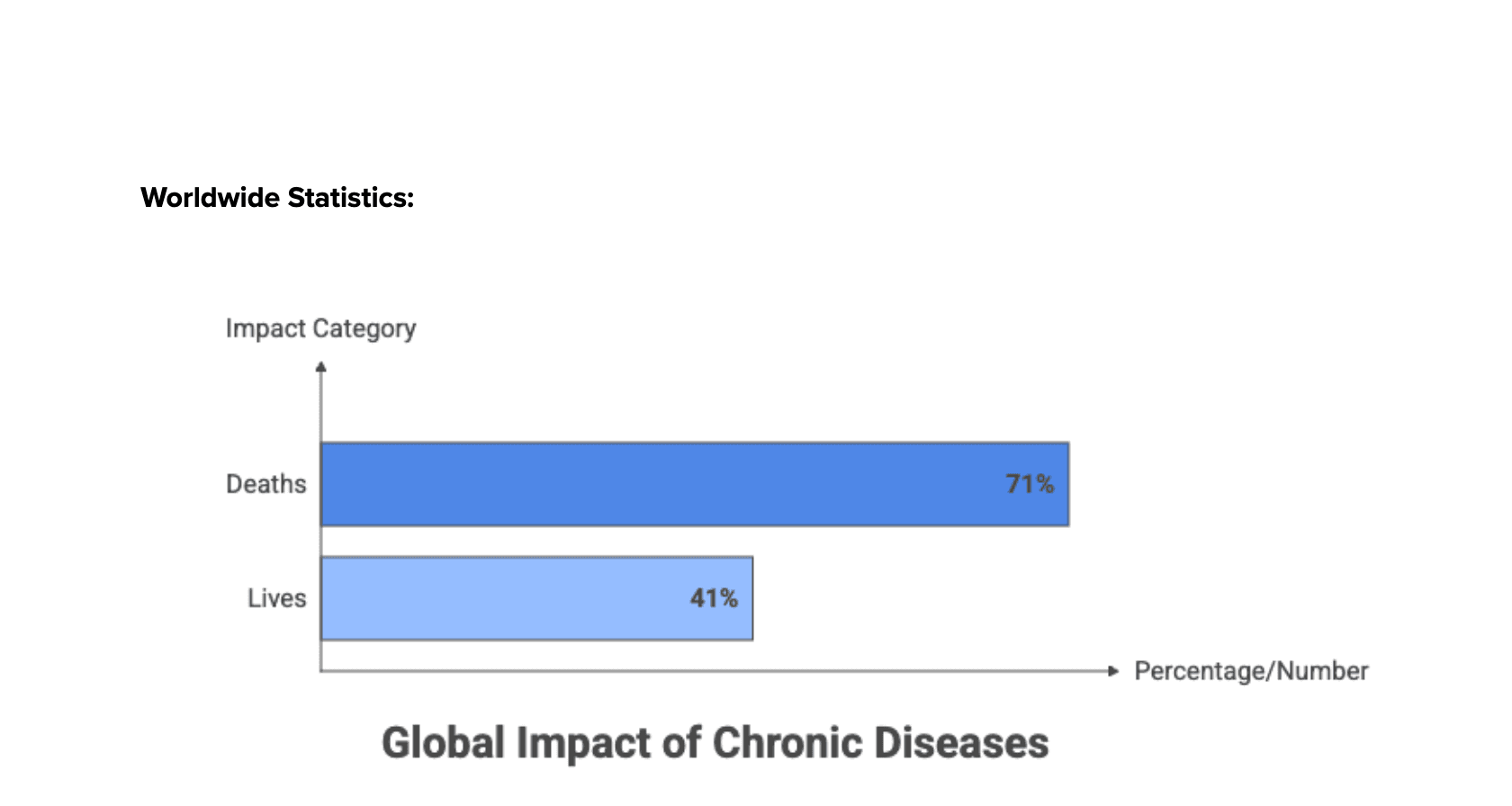
- 71% of all deaths globally attributed to chronic diseases
- 41 million lives claimed annually by chronic conditions
- Rising prevalence in both developed and developing nations
- Increasing burden on healthcare systems worldwide
The Urgency: This staggering prevalence underscores the critical need for proactive management strategies that prevent complications, reduce healthcare costs, and save lives. Dual enrollment programs like CircleHealth's Remote Patient Management offer a scalable solution to this global crisis.
Patient-Centered Care Enhanced by Technology
The Human-Technology Balance
Circle Health's approach recognizes that technology alone cannot solve the chronic disease crisis. The integration of technology with human empathy creates irreplaceable continuity of care that empowers patients while optimizing healthcare resources.
Key Principles:
Technology Enables:
- Continuous physiological monitoring
- Early detection of concerning trends
- Data-driven clinical decision making
- Efficient resource utilization
- Scalable care delivery
Human Touch Provides:
- Emotional support and encouragement
- Personalized education and counseling
- Behavioral intervention and coaching
- Care coordination and advocacy
- Compassionate connection
Together They Create:
- Truly patient-centered care
- Superior clinical outcomes
- Enhanced patient satisfaction
- Sustainable healthcare delivery
- Improved quality of life
Addressing Healthcare Challenges
- Nursing Shortage: Dual enrollment programs optimize care team efficiency, allowing nurses and care coordinators to manage larger patient panels effectively while maintaining high-quality, personalized care through technology-enhanced workflows.
- Healthcare Costs: By preventing complications and reducing hospitalizations, dual enrollment significantly decreases overall healthcare expenditures while improving outcomes—a true win-win for patients and systems.
- Healthcare Access and Equity: Virtual care management programs bridge geographic and transportation barriers, bringing high-quality chronic disease management to underserved populations who might otherwise lack access to specialty care.
Implementation Success Factors
For Healthcare Organizations
Getting Started:
- Identify Target Populations: Focus on patients with poorly controlled chronic conditions who would benefit most from intensive management
- Engage Clinical Champions: Recruit physician leaders who understand and advocate for virtual care programs
- Train Care Teams: Provide comprehensive training on both RPM and CCM program requirements and best practices
- Integrate with EHR: Ensure seamless data flow between monitoring devices, care management platforms, and electronic health records
- Measure Outcomes: Track clinical metrics, patient satisfaction, and financial performance to demonstrate program value
For Care Teams
Best Practices:
- Personalize Interactions: Tailor communication style and care plans to individual patient preferences and needs
- Review Data Before Calls: Prepare for patient interactions by analyzing recent monitoring data and trends
- Set Collaborative Goals: Work with patients to establish meaningful, achievable objectives
- Provide Education: Explain how behaviors and medications affect monitored metrics
- Celebrate Progress: Recognize and reinforce positive changes and achievements
For Patients
Maximizing Benefits:
- Use Devices Consistently: Take readings as prescribed for accurate trend analysis
- Attend Scheduled Check-ins: Participate actively in telehealth visits and phone calls
- Ask Questions: Seek clarification about medications, lifestyle changes, and health data
- Share Concerns: Communicate symptoms, barriers, and challenges openly with care teams
- Engage with Goals: Take ownership of health objectives and track progress
Frequently Asked Questions
What is the difference between RPM and CCM?
RPM (Remote Patient Monitoring) uses connected devices to continuously track physiological data like blood pressure, glucose, and weight. CCM (Chronic Care Management) provides comprehensive care coordination, patient education, and regular human interaction. Together, they create a complete care management program.
Why is dual enrollment more effective than RPM alone?
Dual enrollment combines objective data monitoring with human interaction, behavioral support, medication management, and care coordination. This comprehensive approach addresses both the clinical and lifestyle factors that influence chronic disease, resulting in 50-55% greater improvements in blood pressure control.
Who qualifies for dual enrollment in RPM and CCM?
Patients with chronic conditions requiring ongoing management typically qualify. CCM specifically targets patients with two or more chronic conditions, while RPM benefits anyone with conditions that can be monitored remotely. CircleHealth's team helps determine eligibility based on clinical criteria and insurance coverage.
Is dual enrollment covered by insurance?
Yes. Medicare and most insurance plans cover both RPM and CCM services when medical necessity criteria are met and proper documentation is maintained. CircleHealth handles billing and ensures compliance with all coverage requirements.
How much time commitment is required from patients?
RPM requires brief daily measurements (typically 2-5 minutes) using connected devices. CCM involves scheduled phone or telehealth check-ins, usually 20-30 minutes monthly. Total time commitment is minimal compared to the significant health benefits received.
What chronic conditions benefit most from dual enrollment?
Hypertension, diabetes, heart failure, COPD, chronic kidney disease, and other cardiometabolic conditions show excellent outcomes with dual enrollment. Any chronic condition that can be monitored remotely and benefits from lifestyle modification and care coordination is appropriate.
How quickly can patients expect to see results?
Many patients see measurable improvements within the first month, with substantial progress by three months. The data shows dual enrollment patients achieve target blood pressure control faster than those in RPM-only programs, with sustained improvements over time.
Does CircleHealth provide the monitoring devices?
Yes. CircleHealth provides connected health devices appropriate for each patient's conditions, along with setup support and ongoing technical assistance. Devices automatically transmit data to the care team, eliminating manual recording.
Conclusion: The Future of Chronic Disease Management
The evidence is clear: dual enrollment in Remote Patient Monitoring and Chronic Care Management represents a superior approach to chronic disease management compared to either program alone. Circle Health's integrated Remote Patient Management model achieves dramatically better clinical outcomes—including 50-55% greater blood pressure reductions—while enhancing patient engagement, satisfaction, and quality of life.
As chronic diseases continue to affect nearly half of all Americans and consume the majority of healthcare resources, innovative solutions like dual enrollment become not just beneficial but essential. The strategic combination of technology-enabled monitoring with compassionate human care creates a powerful synergy that addresses the complex, multifaceted nature of chronic disease.
Circle Health remains committed to redefining chronic condition management through this evidence-based, patient-centered approach. By leveraging the complementary strengths of RPM and CCM, we're transforming healthcare delivery into a model that is equitable, efficient, and effective—leaving no patient behind.
The future of healthcare is here, and it's brighter when technology and humanity work together. CircleHealth's dual enrollment programs represent this future, offering transformative care that bridges gaps in access and equity while delivering measurably superior outcomes.
Ready to implement dual enrollment programs at your organization? Contact Circle Health today to learn how our Remote Patient Management solution can transform your chronic disease care delivery and achieve optimal patient outcomes.

