Learn what Principal Care Management (PCM) is, how it works, and why it’s vital under value-based care. Explore benefits, CPT codes, implementation strategies, and best practices for healthcare providers.
Introduction
The U.S. healthcare landscape is shifting rapidly away from reactive, episodic care toward models that emphasize ongoing, proactive management of chronic conditions. With rising prevalence of chronic illness and escalating costs associated with hospitalisations and complications, providers are under pressure to adopt strategies that deliver better outcomes at lower overall cost.
In this context, Principal Care Management (PCM) emerges as a targeted, high-impact approach: it enables providers to dedicate structured, monthly care coordination to patients who have a single, complex chronic condition and face substantial risk of deterioration.
By engaging these patients more intensively between office visits, PCM allows practices to tighten the grip on disease management, prevent avoidable complications, and align more closely with value-based care paradigms.
What is Principal Care Management (PCM)?
Principal Care Management is a Medicare-recognised program designed for patients who have one chronic, highly complex condition that is expected to last at least three months (and often much longer) and which places them at significant risk of hospitalisation, decompensation, functional decline or death.
Under PCM, a provider (or a qualified healthcare professional) oversees a disease-specific care plan and must coordinate care, adjust treatment, and engage the patient monthly — outside of usual face-to-face visits.
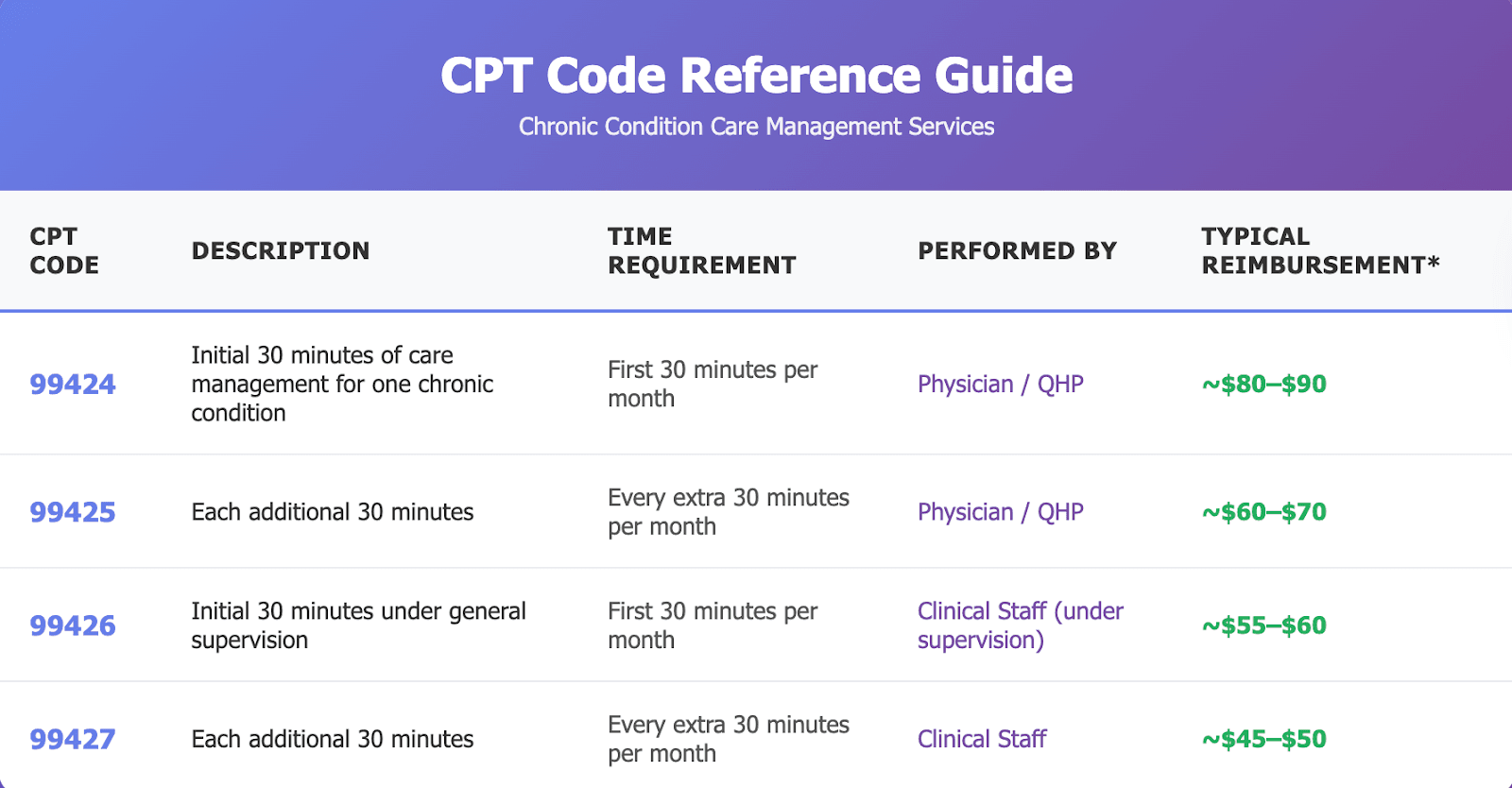
These services are billed using dedicated CPT codes (e.g., 99424/99425 for physician or qualified provider time; 99426/99427 for clinical staff time) that reflect this more intense level of coordination.
Why PCM Was Introduced
Prior to PCM, many care-management models focused on patients with multiple chronic conditions (for example, the Chronic Care Management (CCM) program).
But what about patients who have a single, serious chronic illness (say, advanced heart failure, chronic obstructive pulmonary disease, or end-stage renal disease) who may not meet the “two or more chronic conditions” threshold but still require significant care coordination and risk mitigation? That gap is what PCM addresses.
CMS and other payers recognised that such patients often generate high resource use, and while they did not fit neatly into existing management programs, they clearly benefit from structured monthly oversight.
PCM was introduced to give practices a mechanism to engage these patients—and to be reimbursed for the extra time and coordination required.
Key Features of PCM
- Single-condition focus: Unlike CCM, which requires two or more chronic conditions, PCM focuses on one primary diagnosis for which the patient is being managed.
- Monthly engagement: The care team must spend a minimum of 30 minutes per calendar month (and potentially more) on the management of that condition, beyond usual office visits.
- Comprehensive, disease-specific care plan: During enrolment the provider must create, implement and revise a care plan tailored to the patient’s condition, incorporating goals, treatments, monitoring, and coordination tasks.
- Payment and billing structure: Through CPT codes 99424 / 99425 (for physician/NPP) and 99426 / 99427 (for clinical staff under supervision), PCM is reimbursable under Medicare Part B—and recognises that this kind of care coordination is valuable and billable.
- Alignment with value-based care: Because PCM supports improved outcomes (fewer hospitalisations, better disease control) and stronger patient engagement, it aligns well with population health goals, value-based contracting and alternative payment models.
PCM vs. Chronic Care Management (CCM)
At first glance, Principal Care Management (PCM) and Chronic Care Management (CCM) appear quite similar — both programs reimburse clinicians for providing structured, non-face-to-face care coordination for patients with chronic illnesses. However, there are key distinctions that determine which program a patient qualifies for and how a provider should bill.
1. Number of Chronic Conditions
- PCM: Intended for patients with only one complex chronic condition that significantly threatens health status or poses risk of hospitalization or functional decline.
- CCM: Covers patients with two or more chronic conditions expected to last at least 12 months (or until death), where those conditions collectively place the patient at significant risk.
Example: A patient with advanced congestive heart failure but no other chronic conditions qualifies for PCM.
A patient with both diabetes and chronic kidney disease would fall under CCM.
2. Scope and Focus of Care
- PCM: Focuses on developing and monitoring a disease-specific care plan targeting the single, principal condition.
- CCM: Involves a comprehensive care plan addressing the interplay between multiple comorbidities, medications, and overall health maintenance.
3. Care Team and Oversight
- Both programs can be managed by physicians, qualified healthcare professionals (QHPs), or clinical staff under supervision.
- However, PCM often involves specialists (e.g., cardiologists, pulmonologists, nephrologists) managing one major condition, whereas CCM is typically led by primary care providers who coordinate across specialties.
4. Billing and Time Requirements (with Potential Revenue Insights)
PCM (Principal Care Management) CPT Codes
Potential Monthly Revenue Example:
If a specialist manages 50 patients under PCM (average reimbursement ~$60/patient), that’s approximately $3,000/month in additional recurring revenue.
CCM (Chronic Care Management) CPT Codes
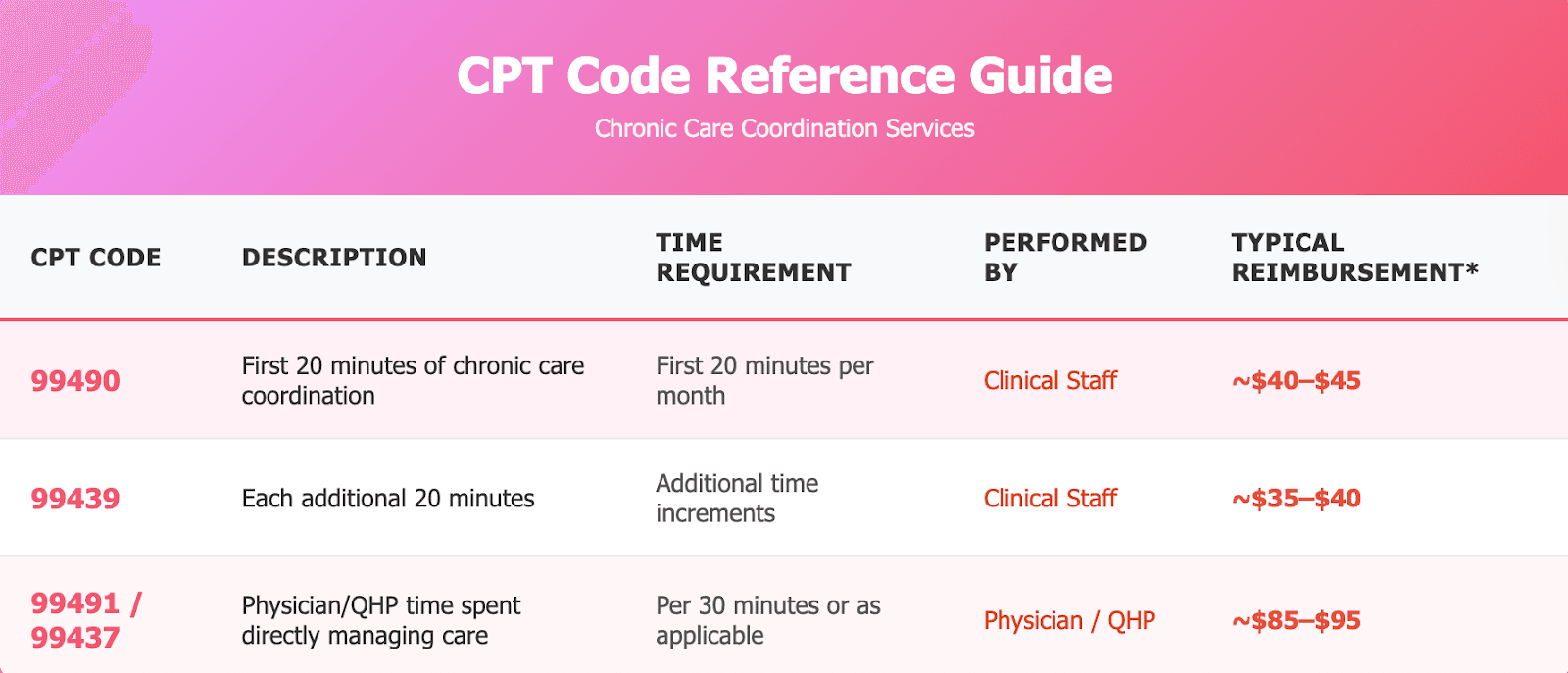
Potential Monthly Revenue Example:
A practice with 100 eligible patients could generate $4,000–$5,000/month through CCM reimbursements.
Compliance Note
A patient cannot be billed under both PCM and CCM in the same month by the same provider.
Practices should select the model that best reflects the intensity and type of care provided during that period.
5. Purpose Within Value-Based Care
- PCM: Encourages specialists to take an active, reimbursed role in longitudinal care, improving continuity and reducing hospital admissions for single high-risk conditions.
- CCM: Enables primary care teams to coordinate across multiple comorbidities, medication management, and preventive care.
In essence: PCM is narrow but deep—intensively managing one condition—while CCM is broad but integrated—overseeing multiple ongoing conditions in a holistic manner.
Who qualifies for PCM? Core Requirements
Understanding eligibility and documentation requirements is key for compliance and reimbursement, as defined by the Centers for Medicare & Medicaid Services (CMS).
1. Patient Eligibility Criteria
A patient is eligible for PCM if they meet all the following conditions:
- The individual has one serious chronic condition expected to persist for at least 3 months or until death.
- The condition poses a significant risk of hospitalization, functional decline, or mortality.
- The patient requires frequent medication adjustments, monitoring, or coordination among multiple care providers.
- The patient has not been enrolled in another care management program (such as CCM) for the same condition in the same billing period.
- The patient has given verbal or written consent for PCM services and understands that cost-sharing may apply under Medicare Part B.
Common qualifying conditions include:
- Congestive Heart Failure (CHF)
- Chronic Obstructive Pulmonary Disease (COPD)
- End-Stage Renal Disease (ESRD)
- Advanced Cancer or Neurological Disorders
- Uncontrolled Diabetes with complications
2. Required Core Elements of PCM Services
To comply with CMS rules and successfully bill PCM codes, the following service components must be in place:
A. Comprehensive Disease-Specific Care Plan
- Must outline patient goals, symptom management strategies, medication adjustments, and follow-up schedules.
- Should be electronically accessible to the patient and care team (via EHR).
- Must be reviewed and updated regularly based on the patient’s progress.
B. Ongoing Communication & Coordination
- Care team must maintain consistent contact with the patient, typically via phone or remote check-ins.
- Communication should extend to specialists, labs, and community providers as needed.
- Documentation of all interactions and time spent is mandatory.
C. Minimum Time Threshold
- Providers or staff must spend at least 30 minutes per month managing the patient’s care.
- Activities can include reviewing test results, updating care plans, coordinating with other providers, or patient education.
D. Patient Consent & Documentation
- Verbal or written consent must be documented before initiating PCM services.
- The patient must be informed about:
- The nature of PCM services,
- That only one provider may bill PCM per month, and
- Any applicable cost-sharing.
- The nature of PCM services,
E. Technology & Accessibility
- Practices should utilize certified EHR or care-management platforms to document, time-track, and communicate with patients.
- Platforms like Circle Healthcare’s system can streamline compliance by automatically tracking care minutes and generating billing reports.
3. Who Can Provide PCM?
According to CMS, PCM can be furnished by:
- Physicians (MD/DO)
- Qualified healthcare professionals (NPs, PAs, CNSs, clinical psychologists where applicable)
- Clinical staff under the supervision of a billing provider
The supervising provider must maintain continuity of care, ensuring that the PCM plan is reviewed and updated monthly.
4. Practical Example
A cardiologist managing a patient with chronic heart failure provides monthly remote check-ins, adjusts diuretics based on symptoms, reviews lab results, and coordinates with the primary care provider.
These activities collectively exceed 30 minutes in a month — making the encounter billable under PCM (CPT 99424 or 99426, depending on who performed the services).
Billing & CPT Codes for PCM
Billing correctly for Principal Care Management (PCM) is critical to ensure compliance and timely reimbursement. CMS introduced specific CPT codes to recognize the additional, non-face-to-face time clinicians dedicate each month to managing a patient’s single complex chronic condition.
A. PCM CPT Codes Overview (2025–2026)
PCM codes are split into two categories based on who delivers the care — the billing provider (physician or qualified healthcare professional) and clinical staff (under direct supervision).
B. Key Billing Rules
- Single Condition Rule:
PCM applies only when the care team manages one qualifying chronic condition expected to last at least three months.
- No Overlapping Programs:
You cannot bill PCM and CCM or PCM and RPM (Remote Patient Monitoring) for the same condition in the same calendar month. However, PCM + RPM can be billed if the RPM focuses on device data management while PCM covers broader care coordination.
- Time-Based Billing:
Each code represents cumulative time spent across the month — reviewing labs, calling patients, updating plans, etc. Documentation must show actual time logged.
- Supervision Requirements:
- 99424/99425: May be billed when performed directly by the billing provider.
- 99426/99427: Must be furnished by clinical staff under general supervision of the billing provider.
- 99424/99425: May be billed when performed directly by the billing provider.
- Documentation Essentials:
- Updated, disease-specific care plan
- Date and time of each activity
- Total time spent during the month
- Patient consent and communication logs
- Updated, disease-specific care plan
- Reimbursement Rates (Approximate 2025 figures):
- 99424: ~$80–$85
- 99425: ~$60
- 99426: ~$60–$65
- 99427: ~$45–$50
(Rates vary by locality and MAC)
- 99424: ~$80–$85
- Billing Frequency:
Each of the above codes may be billed once per calendar month, provided all criteria are met and time thresholds are achieved.
C. Common Billing Mistakes to Avoid
- Submitting PCM and CCM together for the same patient and month
- Not updating the care plan or documenting each communication
- Missing explicit patient consent in records
- Logging time but not specifying the activity performed
- Billing below the minimum 30-minute threshold
Proper use of PCM codes ensures not only reimbursement but also regulatory compliance — protecting practices from denials and audits.
Benefits of PCM for Providers and Patients
Principal Care Management isn’t just a billing opportunity — it’s a strategic approach that strengthens the provider–patient relationship, improves outcomes, and supports the shift to value-based care.
A. Benefits for Patients
- Improved Chronic Disease Control
Regular follow-up and proactive communication reduce flare-ups, medication errors, and emergency visits.
Example: A COPD patient receiving monthly PCM calls experiences fewer exacerbations and hospital admissions.
- Enhanced Engagement & Education
Patients receive continuous coaching and reminders between visits — leading to higher adherence and confidence in self-management.
- Better Access to Care
PCM encourages more touchpoints with the care team, even outside of clinic visits, offering timely interventions and adjustments.
- Continuity and Coordination
The care plan ensures all providers (specialists, pharmacists, primary care) are aligned — preventing duplications and gaps in care.
- Reduced Hospitalizations & ER Utilization
Studies cited by CMS show structured chronic care management can cut hospital readmissions by up to 15–20%, a trend PCM continues by focusing on the most critical single condition.
B. Benefits for Providers and Practices
- Additional Revenue Stream
PCM creates a consistent, billable monthly service — adding incremental income while improving patient outcomes.
Practices that effectively enroll even 100 eligible patients can realize thousands of dollars in recurring revenue monthly.
- Improved Quality Metrics
Consistent follow-up helps providers meet quality measures for Medicare and other value-based contracts — such as medication reconciliation, blood pressure control, or hospital readmission reduction.
- Stronger Specialist Involvement in Value-Based Care
Previously, most care management models (like CCM) favored primary care. PCM empowers specialists — cardiologists, pulmonologists, endocrinologists — to participate directly in value-based programs.
- Workflow Efficiency via Digital Tools
Integrated EHR and care coordination platforms (like Circle Healthcare) streamline documentation, patient tracking, and billing — reducing administrative burden and increasing staff productivity.
- Enhanced Patient Retention and Satisfaction
Regular, structured communication builds trust and loyalty, translating into higher retention rates and stronger patient–provider relationships.
- Alignment with Population Health Goals
PCM supports broader health system aims — early intervention, better outcomes, and lower total cost of care — critical for Accountable Care Organizations (ACOs) and other risk-based arrangements.
C. Real-World Example: How PCM Delivers Results
A pulmonologist manages a patient with moderate COPD. Through monthly PCM calls:
- The nurse checks symptoms, reinforces inhaler use, and updates medication records.
- The physician reviews spirometry trends and modifies therapy accordingly.
- The patient avoids two ER visits in six months due to early intervention.
The result: fewer exacerbations, better control, and a stronger provider-patient relationship — all while generating compliant PCM reimbursement.
How to Implement PCM in Practice
Implementing Principal Care Management (PCM) successfully requires a structured approach that integrates clinical workflows, staff responsibilities, and digital tools. When executed effectively, PCM can deliver measurable patient benefits and sustainable revenue for practices.
Step 1: Identify Eligible Patients
Start by mining your EHR or patient management software for individuals who meet PCM eligibility criteria:
- One serious chronic condition expected to last ≥3 months
- Condition poses significant risk of hospitalization or functional decline
- Frequent medication or monitoring adjustments required
- Not currently enrolled in CCM for the same condition
Examples of eligible conditions:
Heart failure, COPD, ESRD, advanced diabetes with complications, Parkinson’s disease, cancer under ongoing treatment, or post-transplant immunosuppression.
Tip: Use diagnostic codes (ICD-10) and hospitalization history to flag potential PCM candidates. Automate reports monthly for efficiency.
Step 2: Obtain Patient Consent
Before enrollment, obtain verbal or written consent confirming that:
- The patient understands the purpose and benefits of PCM
- Only one provider can bill PCM per calendar month
- Cost-sharing may apply under Medicare Part B
Record this consent in the patient’s EHR with the date, staff initials, and summary of the discussion.
Step 3: Create a Disease-Specific Care Plan
A well-structured care plan is the foundation of PCM. It should include:
- Detailed diagnosis and clinical summary
- Measurable goals (e.g., blood pressure <130/80 mmHg)
- Treatment regimen and medication list
- Monitoring schedule and escalation protocols
- Roles of involved providers (e.g., cardiologist, primary care, pharmacist)
- Patient self-management instructions
Best practice: Keep the plan accessible electronically so patients and all clinicians can view updates in real time.
Step 4: Establish Monthly Follow-Up Protocols
Develop a workflow to ensure each PCM patient receives at least 30 minutes of structured contact monthly. Activities can include:
- Symptom tracking or medication reconciliation
- Reviewing lab results or test reports
- Adjusting therapy plans
- Coordinating with other providers
- Patient education or counseling calls
Assign tasks across the care team — clinical staff handle check-ins, while providers review and approve updates.
Step 5: Track Time and Activities Accurately
CMS requires precise time documentation for PCM billing. Use care-management software to automatically log:
- Start and end times of calls
- Notes on each activity performed
- Total minutes accumulated per patient each month
This ensures compliance and simplifies billing audits.
Step 6: Bill and Review Performance
After the monthly cycle, bill appropriate CPT codes (99424–99427) based on who delivered services and total time logged.
Conduct monthly reviews to track:
- Enrollment numbers
- Patient outcomes (hospitalization rates, adherence)
- Revenue generated
- Staff workload
Circle Healthcare’s platform can automate patient identification, consent tracking, and billing submissions, making PCM implementation efficient and compliant.
Step 7: Monitor and Refine the Program
Evaluate effectiveness quarterly using KPIs:
- Reduced readmissions
- Improved disease metrics (HbA1c, blood pressure, etc.)
- Patient satisfaction scores
- Cost savings under value-based contracts
Refine workflows based on data insights — e.g., optimizing call schedules or expanding PCM to new specialties (cardiology, nephrology, pulmonology).
Common Pitfalls & Compliance Considerations
While PCM is a high-value service model, many practices face denials or audit risks due to documentation gaps or misinterpretations of CMS rules. Avoiding these pitfalls ensures both compliance and financial sustainability.
A. Overlapping Care Management Programs
Issue: Billing PCM for a patient already enrolled in Chronic Care Management (CCM) or Transitional Care Management (TCM) for the same condition during the same month.
Solution:
- Coordinate internally to designate one program per patient per month.
- If a patient transitions from CCM → PCM, document the switch and update the care plan accordingly.
B. Incomplete or Outdated Care Plans
Issue: CMS requires a current care plan reflecting recent progress, interventions, and goals. Many claims fail due to lack of updates.
Solution:
- Review and revise the plan monthly.
- Document every change — medication updates, lab reviews, new goals — with time stamps.
C. Missing Time Documentation
Issue: PCM billing is time-based, and vague notes (“monthly follow-up call”) are not acceptable.
Solution:
- Log exact duration of each contact and activity.
- Use digital timers or automated EHR logging tools.
- Aggregate total minutes before submitting claims.
D. Lack of Patient Consent
Issue: PCM services require explicit consent before billing. Missing consent documentation can result in denied claims or recoupments.
Solution:
- Record verbal consent in the EHR with date and staff name.
- Obtain written consent whenever possible.
- Reconfirm consent annually or when program terms change.
E. Unclear Provider Supervision
Issue: Clinical staff may perform PCM activities, but billing provider supervision is mandatory.
Solution:
- Document supervision type (general vs. direct) in each encounter.
- Ensure billing provider reviews care plans and notes monthly.
F. Poor Communication Between Providers
Issue: Specialists, primary care, and ancillary providers often operate in silos, leading to duplication or gaps.
Solution:
- Designate a PCM lead clinician responsible for central coordination.
- Use shared care-management software or Circle Healthcare’s interoperability features to sync updates automatically.
G. Not Updating Billing Codes or Rules
Issue: CMS periodically revises PCM code definitions and reimbursement rates. Using outdated codes can delay payments.
Solution:
- Review CMS updates annually (especially each January).
- Train billing staff to stay current with new CPT and HCPCS modifiers.
H. Ignoring Quality Metrics
Issue: Focusing solely on billing without tracking outcomes undermines PCM’s purpose.
Solution:
- Align PCM reporting with quality measures like HEDIS or MIPS.
- Track metrics such as medication adherence, ER utilization, and functional status.
I. Inadequate Technology Infrastructure
Issue: Manual PCM tracking is error-prone and time-intensive.
Solution:
- Adopt integrated tools (like Circle Healthcare’s PCM module) that automate:
- Time tracking and billing
- Consent management
- Outcome reporting
- Real-time patient communication
- Time tracking and billing
Compliance Checklist for PCM Success
Patient consent documented
Current disease-specific care plan
Time logs ≥30 min/month
Non-overlapping CCM/TCM enrollment
Monthly provider review
Accurate CPT code selection
Secure documentation storage
Following these best practices ensures smooth audits, consistent reimbursement, and stronger patient trust — allowing your PCM program to thrive within a compliant, value-based framework.
Implementing a Principal Care Management Program in Your Practice
Implementing a PCM program requires strategic planning, coordination, and adherence to compliance standards. Healthcare providers should begin by identifying eligible patients—those with a single high-risk chronic condition expected to persist for at least three months. Common examples include congestive heart failure, diabetes, COPD, or severe asthma.
Key Steps in Implementation
- Assess Patient Eligibility
Use electronic health records (EHR) and risk stratification tools to identify patients with a single complex chronic condition that significantly impacts their daily lives.
- Establish Clinical Workflows
Define team responsibilities, such as assigning a care manager, setting communication protocols, and scheduling follow-up check-ins. Integration with telehealth and remote monitoring tools helps streamline these processes.
- Use Certified Technology Platforms
Implement a HIPAA-compliant digital care management system for secure documentation, billing, and patient engagement. Platforms like ThoroughCare and CareSimple can support PCM documentation and reporting.
- Engage Patients Effectively
Educate patients about the benefits of PCM, how it helps manage their condition, and what to expect in ongoing follow-ups. Strong patient engagement leads to better adherence and improved outcomes.
- Ensure Billing Compliance
Proper documentation is essential to justify CPT codes such as G2064 and G2065. Practices should ensure time-tracking, consent documentation, and electronic health record integration to maintain audit readiness.
Measuring Success in Principal Care Management
The success of a PCM program depends on measurable outcomes across clinical, financial, and patient experience metrics.
Key Performance Indicators (KPIs)
- Clinical Outcomes: Reduction in hospitalizations, emergency visits, and acute episodes for targeted chronic conditions.
- Patient Engagement: Improved appointment adherence and increased communication frequency between patients and care managers.
- Cost Savings: Decrease in total cost of care per patient through proactive management and early intervention.
- Provider Efficiency: Reduced administrative workload and better time management for physicians due to coordinated care workflows.
- Patient Satisfaction: Improved feedback scores reflecting a more supportive and personalized care experience.
Continuous Improvement
Successful PCM programs leverage analytics to identify trends, optimize workflows, and refine intervention strategies. Regularly reviewing program data helps ensure compliance and supports ongoing alignment with value-based care objectives.
Challenges in Principal Care Management and How to Overcome Them
While Principal Care Management offers immense benefits for both providers and patients, implementing and maintaining an effective program isn’t without challenges. Understanding these barriers and proactively addressing them can significantly enhance program success.
Common Challenges
- Identifying Eligible Patients
Many practices struggle to accurately identify patients who meet PCM eligibility criteria. Since PCM targets those with a single high-risk chronic condition, differentiating between patients suited for PCM and Chronic Care Management (CCM) can be tricky.
- Documentation and Compliance Burden
PCM billing requires precise documentation—tracking time spent, obtaining patient consent, and maintaining ongoing communication logs. Missing any element can lead to claim denials or compliance risks.
- Patient Engagement Barriers
Some patients may be hesitant to enroll or fail to see the value of care coordination services, especially when they don’t understand how PCM differs from regular follow-ups.
- Technology Integration Issues
Without seamless integration between EHR systems, telehealth platforms, and billing software, data silos can hinder care coordination and reporting accuracy.
- Resource and Staffing Constraints
Smaller practices often lack dedicated care coordinators or administrative staff to manage PCM processes efficiently.
How to Overcome These Challenges
- Automate Eligibility Screening: Use AI-powered analytics or EHR-integrated tools to automatically flag eligible patients based on diagnosis and risk scores.
- Leverage Digital Documentation Tools: Adopt PCM platforms that streamline compliance, automatically track time, and generate audit-ready reports.
- Educate Patients Early: Use patient-friendly materials or digital onboarding sessions to communicate the benefits and expectations of PCM.
- Integrate Systems Efficiently: Choose interoperable solutions that sync with your existing EHR and telehealth tools.
- Outsource or Partner Strategically: Collaborate with third-party care management partners who can handle PCM workflows and compliance, reducing in-house workload.
Best Practices for Maximizing PCM Effectiveness
Implementing Principal Care Management successfully requires more than meeting compliance standards—it demands strategic execution to ensure long-term effectiveness. Below are actionable best practices to help healthcare organizations maximize the impact of their PCM programs.
1. Standardize Care Protocols
Establish consistent, evidence-based care protocols across your organization. This ensures that every patient with a qualifying chronic condition receives the same high-quality, proactive care experience—irrespective of the provider.
2. Prioritize Communication and Continuity
Effective PCM relies on timely, transparent communication. Regular follow-ups, care plan updates, and collaborative discussions between specialists and patients foster trust and adherence to treatment goals.
3. Leverage Data Analytics
Use advanced analytics to track outcomes, identify care gaps, and optimize intervention timing. Analytics-driven insights can reveal which patient populations benefit most from PCM and where care coordination improvements are needed.
4. Train and Empower Care Teams
Invest in continuous education for care coordinators and clinicians. Ensure your team is proficient in using digital care platforms, understands documentation workflows, and remains updated with the latest PCM billing codes and regulations.
5. Integrate Multi-Disciplinary Collaboration
Encourage collaboration between specialists, primary care providers, and ancillary service teams. This holistic approach enhances patient management, reduces care fragmentation, and supports overall well-being.
Why Principal Care Management Matters in the Value-Based Care Era
The healthcare landscape is rapidly evolving, moving away from fee-for-service models toward value-based care frameworks that reward outcomes rather than volume. In this context, Principal Care Management has emerged as a cornerstone of modern chronic care delivery.
Driving Value in Patient Outcomes
By focusing on a single high-risk condition, PCM enables early intervention, personalized management, and continuous engagement—directly contributing to improved health outcomes and patient satisfaction.
Reducing Healthcare Costs
Proactive management helps reduce hospital readmissions, emergency department visits, and other high-cost interventions. This cost efficiency benefits not only payers and providers but also the healthcare system at large.
Supporting Provider Incentives
Under value-based care arrangements, providers are incentivized for measurable improvements in patient health. PCM aligns perfectly with these goals—delivering quantifiable results through ongoing monitoring and timely intervention.
Empowering Patients Through Education and Technology
PCM programs give patients access to digital tools and regular communication channels that foster better self-management and stronger engagement with their healthcare teams.
Final Thoughts
Principal Care Management is no longer optional—it’s essential. For healthcare providers aiming to thrive under value-based care, PCM offers a scalable, data-driven pathway to improved outcomes, reduced costs, and enhanced patient satisfaction. With the right technology and strategy, Circle Healthcare and similar organizations can lead the transformation toward proactive, patient-centered care.

