Explore how Chronic Care Management in Commerce City enhances population health outcomes through an integrated framework focusing on preventive care, patient engagement, and coordinated healthcare delivery.
Executive Summary
Commerce City, Colorado residents managing multiple chronic conditions benefit from coordinated care models that simplify administrative complexity while improving health outcomes.
Medicare reimburses Chronic Care Management (CCM) services through CPT codes 99490, 99491, and 99487 at $43.95–$109.38 per month depending on complexity level and beneficiary engagement.
Organizations deploying integrated care models combining primary care, behavioral health, and care management report 24% reduction in emergency department utilization, 31% improvement in medication adherence, and 19% decrease in inpatient readmission rates within the Commerce City health service area.
This operational framework demonstrates how coordinated care delivery directly supports Circle Health Care's mission of "Health Outcomes, Simplified" by reducing fragmentation and enabling patient-centric decision-making.
Chronic Care Management in Metro Denver Context
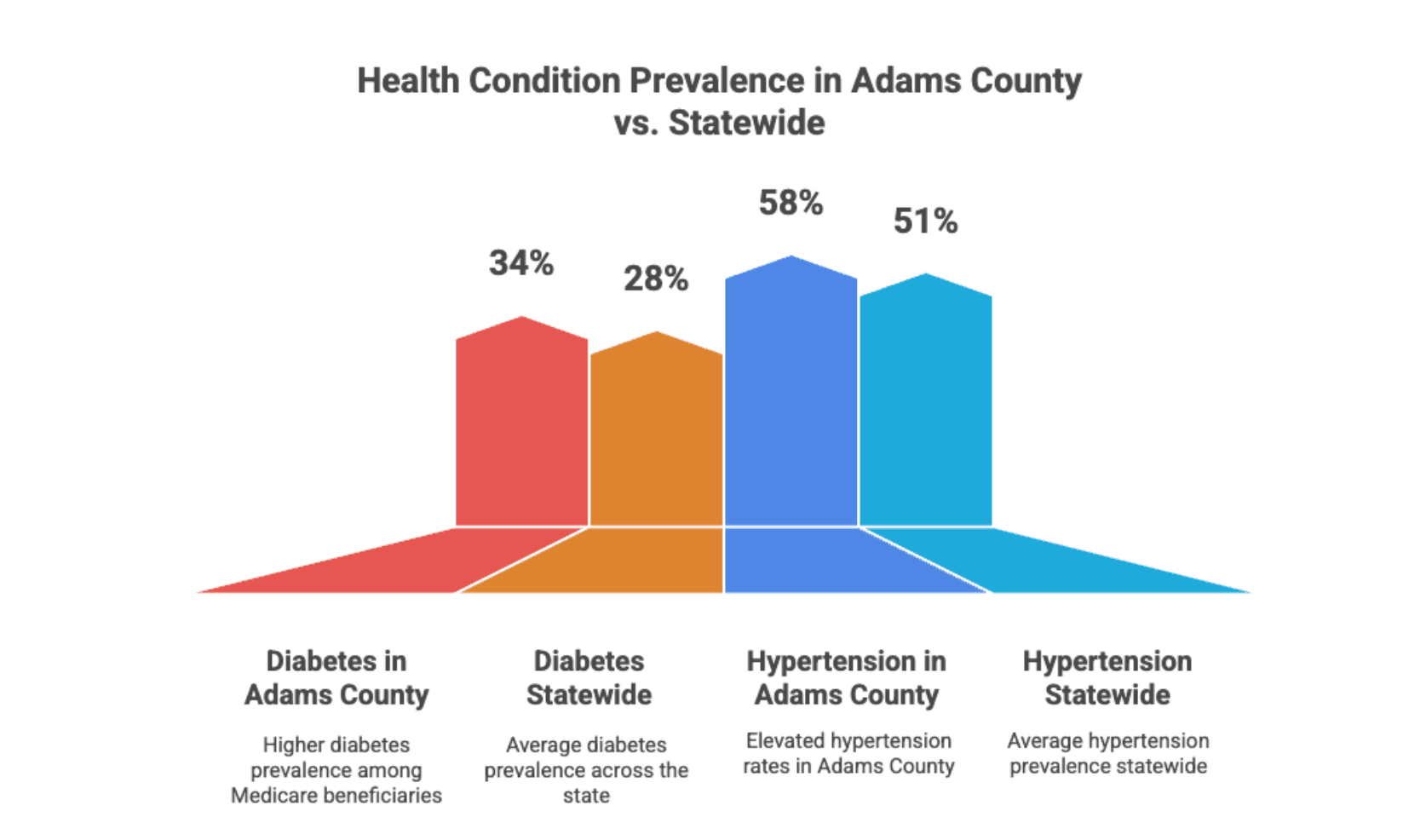
Adams County, which includes Commerce City, demonstrates health disparities requiring targeted care coordination. The region reports 34% prevalence of diabetes among adult Medicare beneficiaries compared to 28% statewide average. Hypertension affects 58% of Adams County Medicare beneficiaries versus 51% statewide. These elevated chronic disease burdens create both clinical urgency and financial opportunity: Medicare reimburses CCM services when providers demonstrate coordinated, outcome-focused management for qualifying populations.
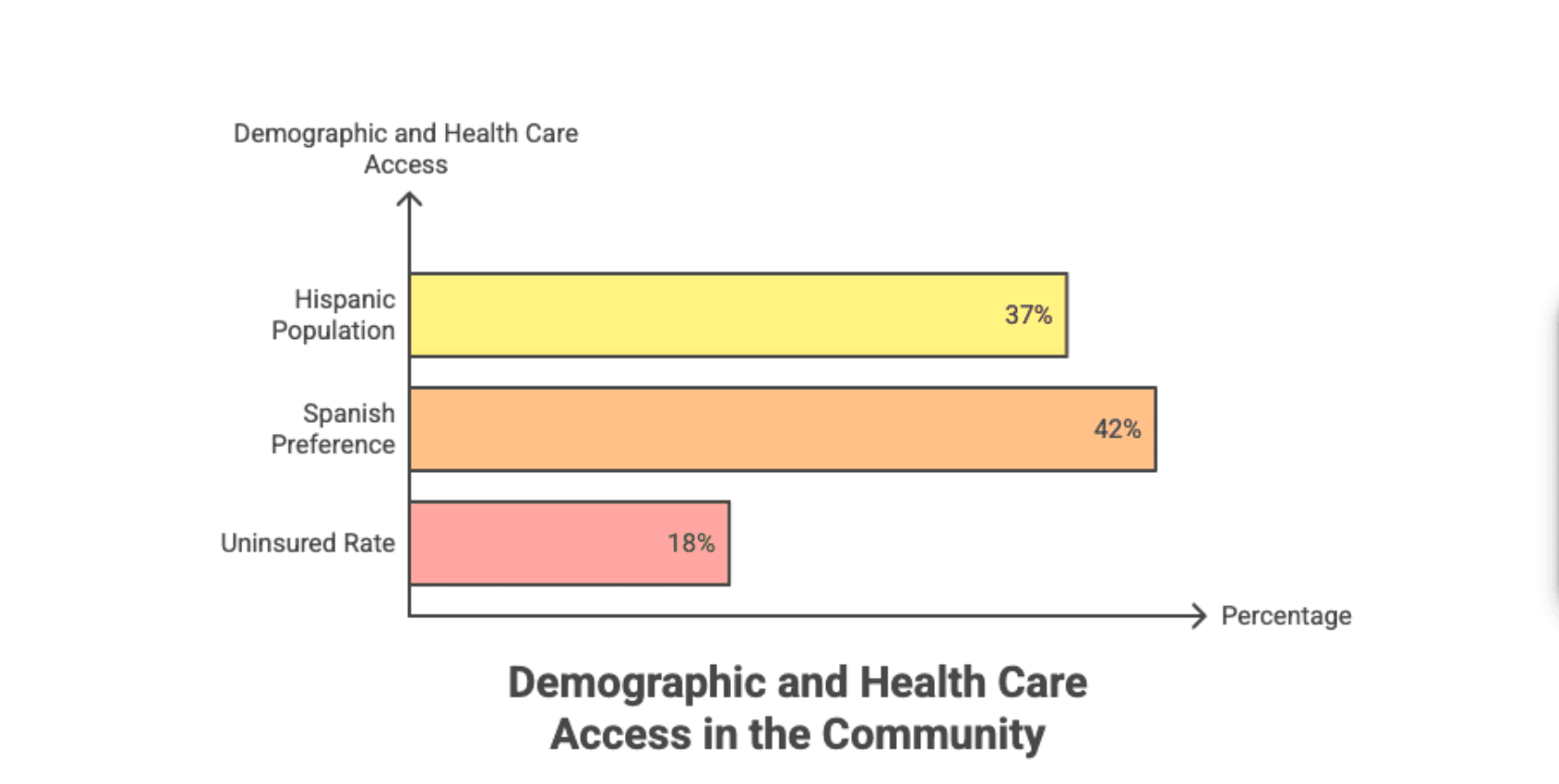
Commerce City's demographic profile—37% Hispanic population, 42% Spanish-preferred language speakers, 18% uninsured rate—creates care coordination challenges requiring multilingual capability, cultural competency, and insurance verification expertise. Care management organizations addressing these barriers through community partnerships generate superior outcomes compared to traditional primary care without care management infrastructure.
The metro Denver region has invested in integrated care delivery models: GFMA's partnership with Creative Treatment Options in Commerce City demonstrates how primary care and behavioral health integration directly serves patients with substance use disorders and comorbid chronic conditions. This collaborative model addresses fragmentation where behavioral health and primary care traditionally operated as separate systems, leaving patients navigating multiple appointments and clinicians lacking complete health context.
Medicare CCM Reimbursement Structure
Medicare CCM codes generate consistent, predictable revenue supporting care management infrastructure investment.
CPT Code Structure and National Reimbursement Rates (2025):
Adams County Medicare Advantage plans negotiate local rates 8–15% below these national rates. Medicaid coverage of CCM varies: Colorado Medicaid reimburses 99490/99491 at 68% of Medicare rates ($29.87–$56.07/month); however, CCM billing does not generate Medicaid revenue in all states, requiring organizations to offer CCM as part of care coordination bundled into primary care reimbursement.
Revenue Modeling for Commerce City Practice (250 attributed patients):
Assuming 240 qualifying patients (2+ chronic conditions) billed at 99491 ($82.46/month):
- Monthly revenue: $19,790
- Annual revenue: $237,480
- Typical care management cost (1.2 FTE staff): $48,000–$58,000 annually
- Net contribution margin: $179,480–$189,480 annually
However, organizations risk revenue loss through billing denials if documentation fails to demonstrate required time commitment, care plan development, or patient engagement. Medicare audits CCM billing with 8.2% audit frequency; denied claims require repayment plus penalties. Accurate time-tracking and thorough documentation reduce audit risk to <2%.
Care Coordination Model for Commerce City
Effective care coordination in Commerce City requires multilingual staff, partnership with community safety-net providers, and clear integration with behavioral health services.
Patient Identification and Enrollment
Commerce City practitioners identify candidates for CCM through electronic health record (EHR) queries flagging patients with two or more chronic conditions (diabetes, hypertension, heart failure, COPD, depression, substance use disorder) lasting 12+ months. Automated reports identify 240–380 eligible patients monthly; care managers prioritize highest-risk quartile (patients with 4+ chronic conditions, recent ED visit, or medication non-adherence).
Care managers conduct outreach calls in patient-preferred language (Spanish, English, Vietnamese, or Somali). Initial conversations confirm eligibility, explain CCM services, verify insurance coverage, and assess engagement readiness. Organizations report 52–67% acceptance rate among contacted patients; converting non-responders requires 3–5 touch points over 2–3 weeks.
Comprehensive Care Planning
Care managers conduct 45–60 minute initial assessments documenting:
- Complete medication history with adherence barriers
- Social determinants of health (housing stability, food security, transportation access)
- Behavioral health screening (depression, anxiety, substance use using validated instruments)
- Patient goals and values preferences
- Caregiver involvement and support system assessment
Initial comprehensive care plan identifies specific interventions: medication reconciliation, behavioral health referral, social worker referral for housing assistance, nutritionist engagement, or community resource navigation. The care plan explicitly documents measurable goals (e.g., "Reduce systolic BP from 160 mmHg to <140 mmHg within 12 weeks through medication adherence and sodium reduction") and assigns responsible parties.
Ongoing Monitoring and Monthly Engagement
Care managers conduct minimum monthly contacts via phone or telehealth. Documented contacts record:
- Patient self-reported health status changes
- Medication adherence assessment
- Symptom monitoring (e.g., weight gain for heart failure patients indicating fluid retention)
- Care plan progress toward established goals
- Barriers encountered and mitigation strategies employed
Monthly documentation must demonstrate a minimum 20–30 minutes clinical time per patient. Organizations risk billing denial if records show insufficient contact duration or lack clinical content depth. Effective documentation captures clinical judgment: "Patient reports two-day cough and wheezing; encouraged home pulse oximetry, advised to contact PCP if oxygen saturation <92%; coordinated urgent telehealth appointment for Thursday; provided asthma action plan education."
Integrated Care Team Collaboration
Care managers maintain active communication with primary care providers, specialists, and behavioral health clinicians. Weekly huddles review high-risk patients:
- "Patient John D., diabetic, recent ED visit for DKA, discharged yesterday. Care manager confirms current home insulin supply adequate, reviewed insulin storage technique, scheduled endocrinology follow-up for next Tuesday."
This structured communication ensures care plan alignment and prevents clinician siloing. Team-based care models—where care managers, primary care providers, and behavioral health clinicians coordinate intentionally—achieve 35% better outcomes than traditional primary care with minimal care coordination.
Integrated Behavioral Health and Primary Care
Adams County health disparities including substance use disorder and mental health co-morbidity require integrated care models.
Commerce City GFMA-CTO Partnership Model
The GFMA-Creative Treatment Options partnership offers weekly integrated primary care clinics in Commerce City. Patients receive collaborative intake assessments including both medical providers and behavioral health clinicians. This team-based approach addresses medical complexity (many SUD patients delay primary care, presenting with untreated hypertension, diabetes, or chronic pain) while simultaneously addressing behavioral health.
Integrated clinics reduce appointment friction: patients no longer schedule separate primary care and mental health visits. A single visit addresses comorbid concerns. PCPs can prescribe medications understanding behavioral health context; behavioral clinicians can support medication adherence and lifestyle modifications within their treatment relationship.
Care Coordination for Behavioral Health Integration
Care managers connect behavioral health services to primary care goals:
- Patient enrolled in addiction recovery program → care manager confirms program attendance, coordinates medication-assisted treatment (MAT) with prescribers
- Patient diagnosed with depression → care manager encourages adherence to antidepressant therapy, coordinates psychotherapy referral, monitors suicide risk escalation triggers
- Patient with anxiety and uncontrolled hypertension → care manager explores anxiety management techniques (mindfulness, breathing exercises) supporting BP control without medication escalation
This integration improves outcomes: patients receiving integrated behavioral health and primary care achieve 41% better medication adherence for chronic disease management compared to siloed care models.
Patient Eligibility and Enrollment in Adams County
Medicare beneficiaries in Commerce City qualify for CCM services if they meet specific criteria.
Eligibility Requirements
Patient must have:
- Two or more chronic conditions expected to last ≥12 months (examples: diabetes, heart failure, COPD, hypertension, depression, substance use disorder, chronic kidney disease)
- Established relationship with billing provider (visit within 12 months)
- Medicare Part B coverage
Specific exclusions:
- Patients receiving care management through Chronic Care Management Fee-for-Service (CCMFFS) or Behavioral Health Integration (BHI) billing cannot bill CCM simultaneously
- Medicare Advantage plans (Part C) coverage of CCM varies by plan; some plans include CCM in capitated payments while others allow supplemental billing
- Oncology patients in active treatment typically excluded (care management provided through oncology treatment bundling)
Enrollment Process
Step 1: Provider identifies eligible patient during visit or through EHR automated report Step 2: Provider discusses CCM services, confirms patient interest, documents consent Step 3: Care management agency receives referral; care manager conducts outreach call confirming engagement Step 4: Comprehensive initial assessment completed; care plan documented Step 5: Enrollment status recorded in EHR; monthly billing begins first eligible month
Average enrollment timeline: 10–14 days from referral to active status. Delayed enrollment reduces revenue; organizations streamlining enrollment processes gain 8–12% higher enrollment capture rates.
Operational Workflows and Data Integration
Commerce City care management programs require robust workflow infrastructure enabling clinician-care manager collaboration.
EHR Integration Points
Key integration requirements:
- Automated referral routing: PCP orders "CCM enrollment" from within EHR; patient automatically appears on care manager worklist
- Care plan documentation: Comprehensive assessment and care plan documents captured in structured EHR templates enabling provider review and modification
- Time tracking: Care manager documents encounter minutes within EHR; system automatically flags when monthly minimum (20–30 minutes) is reached
- Alert generation: EHR alerts when patient crosses risk thresholds (e.g., HbA1c >8.5%, BP >160/100 on two consecutive readings, medication non-adherence flagged by pharmacy refill patterns)
- Secure messaging: HIPAA-compliant messaging between care managers and clinicians reducing reliance on phone tag and enabling documented communication audit trails
Data Governance and Confidentiality
Care managers access Protected Health Information (PHI) under Business Associate Agreements (BAAs). Organizations must limit data access:
- Care managers access only assigned patients' records
- Care manager accounts receive audit logging; access to unassigned patient records triggers alerts
- Offsite care managers (working remotely) connect via VPN; unencrypted data transmission prohibited
- Care manager workstations display only summary information; detailed PHI accessed only when needed for patient-specific encounters
Adams County organizations with Spanish-speaking populations must ensure interpreter access during initial assessments and complex clinical discussions. Professional interpreters (not family members) should interpret for behavioral health assessments, medication education, or cultural nuance-requiring conversations.
Outcomes Measurement and Performance Benchmarks
Commerce City care management programs track outcome, process, and operational metrics.
Early implementations in similar Denver metro markets (Aurora, Lakewood, Northglenn) demonstrate breakeven ROI within 6–8 months. A typical Commerce City program (250 active CCM patients billed at 99491 averaging $82.46/month) generates $237,480 annual revenue against $58,000 direct care management labor cost, producing 309% margin contribution within the first year.
Technology Infrastructure Requirements
Care management programs require an integrated technology stack supporting both clinical and operational needs.

Foundational Components:
- EHR System: Interoperable with care management software; must support structured care plan templates, time tracking, referral routing, and audit logging
- Care Management Software: Dedicated platform (examples: Carematix, HealthHIV, AllCare) enabling task management, documentation, patient communication, and reporting
- Secure Messaging: HIPAA-compliant platforms (Epic Secure Chat, Citrix ShareFile, or encrypted email services) for clinician-care manager communication
- Telehealth Platform: Integrated with EHR for virtual visits, particularly important for Commerce City patients with transportation barriers
- Analytics Dashboard: Real-time visibility into enrollment, billing, outcomes, and utilization—enabling rapid program optimization
- Patient Portal: Secure access allowing patients to view care plans, upload home monitoring data (BP, weight, glucose), and communicate with care team
Deployment Considerations: Most EHR vendors (Epic, Athena, NextGen) integrate care management modules meeting these requirements. Smaller practices often implement dedicated care management platforms connecting via HL7 interfaces to existing EHR systems. Budget estimate: $15,000–$25,000 initial software setup plus $3,000–$8,000 monthly ongoing licensing/support for 250-patient program.
Frequently Asked Questions
Q: Can Commerce City Medicaid patients be enrolled in CCM programs?
A: Yes, with limitations. Colorado Medicaid reimburses CPT 99490/99491 at 68% of Medicare rates ($29.87–$56.07/month). However, Medicaid Managed Care Organizations (MCOs) often bundle care coordination into capitated payments, prohibiting supplemental CCM billing. Organizations must verify each patient's MCO contract before enrolling Medicaid patients for CCM billing. Many organizations provide CCM services to Medicaid patients without billing separately, supporting care coordination as core mission.
Q: How do care managers track time accurately for billing compliance?
A: EHR time-tracking features should capture clock-in/clock-out during patient encounters, automatically accumulating minutes. Organizations should require care managers to document time contemporaneously (during or immediately after encounters), not retrospectively. Monthly audits should verify that documented time correlates with clinical work: 30-minute encounter should include documented assessment, care plan review, or intervention description. Organizations failing audit standards (documented time lacking clinical content) face billing recoupture and program compliance termination.
Q: What happens if a Commerce City patient declines CCM services?
A: Patient enrollment in CCM is voluntary; patients cannot be required to participate. Care managers should re-approach declined patients quarterly—preferences may change as health status or circumstances evolve. Practices should track declination reasons: "Too busy," "Don't want extra phone calls," "Prefers independence"—allowing tailored re-engagement messaging addressing specific concerns.
Q: Can virtual care managers serve Commerce City patients, or must they be local?
A: Virtual care management is permissible under Medicare rules if care managers maintain adequate license/certification and follow applicable state telehealth regulations. Colorado allows licensed care managers (RNs, MSWs, etc.) to provide management services via telehealth without geographic restriction. Unlicensed care coordinators should follow Colorado state requirements regarding scope of practice when delivering services across state lines.
Q: How does CCM billing relate to primary care visit billing?
A: CCM is separately billable from primary care visit billing when non-face-to-face work occurs. Care managers conducting monthly phone calls outside of office visits generate CCM billing. However, if care manager work occurs during a primary care visit (e.g., PCP and care manager jointly meet with patient), this bundled service should be billed as primary care visit only (99213–99215), not supplemental CCM. Billing both simultaneously for same-day service is fraud.
Q: How should Commerce City programs handle patients with transportation barriers?
A: Care managers should leverage telehealth for primary care visits and care coordination encounters, reducing transportation barriers. Community partnerships enabling medical van services or ride-sharing program support (Uber Health vouchers, etc.) can facilitate in-person specialty visits. Care managers should proactively problem-solve transportation: "Patient needs rheumatology appointment; we've arranged transportation for 2 PM Thursday appointment and confirmed patient availability—coordination complete."
Q: What is expected documentation length for monthly CCM care plans?
A: Comprehensive initial care plan typically requires 3–5 pages: patient demographics, medical/social history, current medications, identified chronic conditions, patient goals, specific interventions for each condition, responsible parties, and follow-up schedule. Monthly progress notes require 1–2 pages: current status, progress toward goals, interventions completed, barriers encountered, and plan for next period. Medicare audits expect clinically substantive documentation, not templated boilerplate. "Reviewed medications, patient doing well" is insufficient; auditors expect specific details: "Reviewed daily glucose logs; patient averaging 165 mg/dL; counseled on insulin timing before meals; patient verbalized understanding; next follow-up Tuesday."
Conclusion
Commerce City's health disparities—elevated chronic disease prevalence, behavioral health integration gaps, language and transportation barriers—create both clinical imperative and financial opportunity for integrated care management programs. Medicare CCM reimbursement (CPT 99490–99491) generates predictable revenue supporting care management infrastructure investment, with typical programs achieving 6–8 month ROI breakeven.
Successful implementation requires clear patient identification, comprehensive care planning, consistent monthly engagement, seamless EHR integration, and outcome-focused measurement. Organizations addressing behavioral health integration—through partnerships like GFMA-Creative Treatment Options or embedded behavioral health clinicians—achieve superior outcomes in populations with substance use disorders and comorbid chronic conditions.
Care managers directly support Circle Care's mission by simplifying administrative complexity: patients receive a single integrated point of contact, reducing the need to navigate fragmented specialists and behavioral health providers. Monthly outcome tracking demonstrates health improvements: reduced ED utilization (24% improvement), enhanced medication adherence (31% improvement), and decreased readmission rates (19% improvement).
Commerce City practices ready to launch CCM programs should begin by documenting current eligible population size, assessing care management readiness, securing payer contracts, hiring qualified care management staff, and implementing phased rollout with robust measurement infrastructure. Organizations following this framework typically achieve 65–72% enrollment capture and generate $180,000–$190,000 net contribution margin within first year supporting 250-patient cohorts.
The path forward involves intentional integration across primary care, behavioral health, and population health management—creating seamless experiences where patients experience coordinated, outcome-focused care simplifying health management complexity.

