Explore 10 ways comprehensive care management services drive value-based care success. Learn how coordinated care solutions improve patient outcomes and reduce costs.
The healthcare industry's shift from fee-for-service to value-based care models requires fundamental changes in how organizations deliver and coordinate patient care. Success in value-based arrangements depends on improving patient outcomes while controlling costs—a challenging balance that demands sophisticated care management strategies.
Comprehensive care management services provide the infrastructure, processes, and team support necessary to thrive under value-based payment models. These services transform fragmented care delivery into coordinated, proactive systems that enhance quality metrics, reduce unnecessary utilization, and ultimately improve patient health outcomes.
Here are ten essential ways that robust care management services enable healthcare organizations to succeed in value-based care arrangements.
1. Proactive Identification of High-Risk Patients
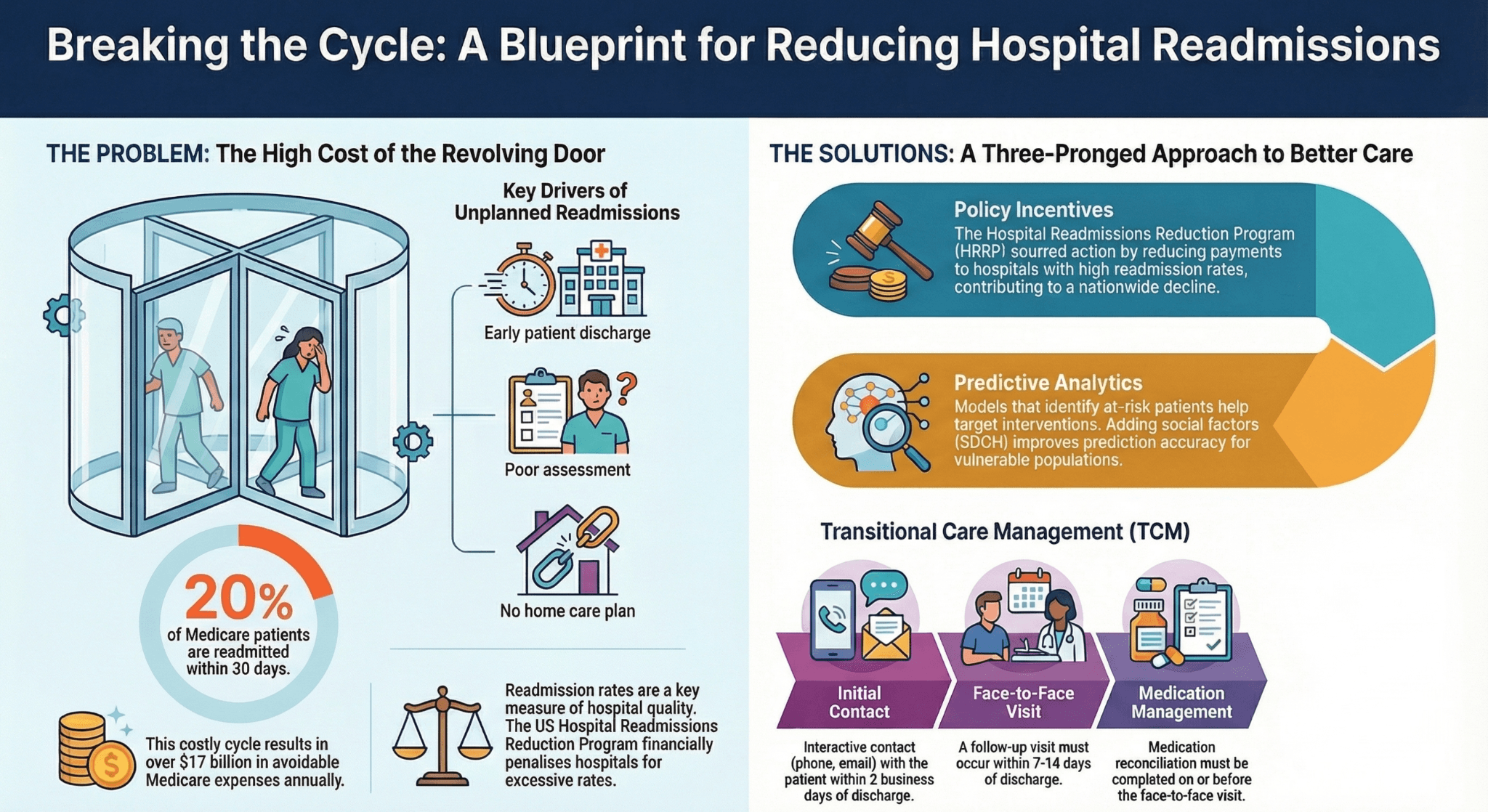
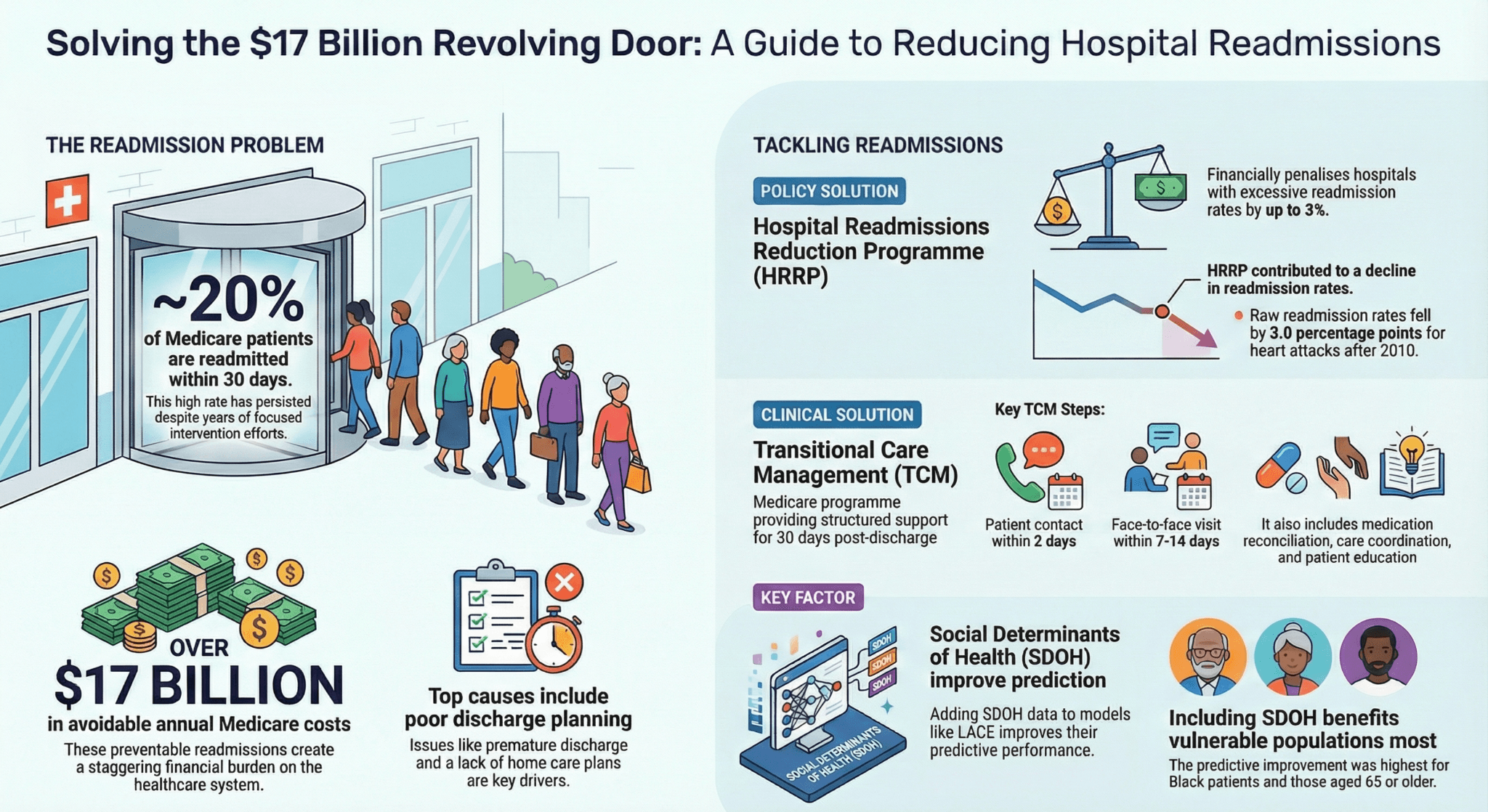
Value-based care success hinges on preventing complications before they become costly. Care management services utilize sophisticated risk stratification algorithms that analyze clinical data, claims history, social determinants, and behavioral factors to identify patients most likely to experience adverse events or high utilization.
Early identification allows care teams to intervene before problems escalate. High-risk patients receive enhanced monitoring, frequent touchpoints, and targeted interventions designed to prevent emergency department visits, hospitalizations, and disease progression. This proactive approach directly impacts the total cost of care while improving patient quality of life.
Modern care management services leverage predictive analytics and real-time data integration to continuously update risk scores, ensuring care teams focus resources where they'll have maximum impact on both patient outcomes improvement and cost containment.
2. Coordinated Care Solutions Across the Continuum
Patients with complex conditions interact with multiple providers, specialists, facilities, and services. Without coordination, this fragmented care leads to duplicated tests, conflicting treatment plans, medication errors, and gaps in follow-up—all of which undermine value-based care objectives.
Comprehensive care management establishes a single source of coordination, ensuring all team members work from a unified care plan. Care managers facilitate communication between primary care, specialists, hospitals, home health agencies, and community resources, creating seamless transitions across care settings.
This coordinated approach reduces redundancies, prevents medical errors, ensures appropriate utilization of services, and creates a cohesive patient experience. For value-based care arrangements, effective coordination directly translates to better quality scores and lower total costs.
3. Chronic Disease Management and Prevention
Chronic conditions account for approximately 90% of healthcare spending and represent the primary focus of most value-based care contracts. Effective care management services implement evidence-based protocols for managing diabetes, heart failure, COPD, hypertension, and other prevalent chronic diseases.
Care managers work with patients to optimize medication adherence, monitor key clinical indicators, promote lifestyle modifications, and ensure completion of preventive screenings. Regular patient engagement helps identify early warning signs of exacerbations, enabling timely interventions that prevent hospitalizations.
By helping patients manage chronic conditions effectively, care management services improve clinical quality measures that determine success in value-based contracts while simultaneously reducing acute care utilization and associated costs.
4. Enhanced Patient Engagement and Activation
Engaged patients who actively participate in their care achieve better outcomes and lower costs—critical factors in value-based care success. Care management services employ various strategies to increase patient engagement, including personalized education, shared decision-making, goal-setting collaboration, and regular motivational support.
Care managers build trusted relationships with patients, understanding their preferences, barriers, and motivations. This relationship enables care team support that resonates with individual patients rather than applying one-size-fits-all approaches. Activated patients are more likely to attend appointments, follow treatment plans, communicate concerns early, and make health-promoting behavioral changes.
Technology platforms supporting care management facilitate patient engagement through convenient communication channels, educational resources, remote monitoring capabilities, and self-management tools that empower patients between clinical encounters.
5. Medication Management and Adherence Support
Medication non-adherence costs the healthcare system billions annually and directly undermines value-based care objectives. Care management services address this challenge through comprehensive medication management programs that identify adherence barriers, provide patient education, simplify complex regimens when possible, and connect patients with financial assistance programs.
Care managers conduct regular medication reconciliation, particularly after care transitions, to prevent errors and ensure therapeutic appropriateness. They also monitor for adverse effects and drug interactions, collaborating with pharmacists and physicians to optimize medication regimens.
Improved medication adherence leads to better chronic disease control, fewer complications, reduced emergency department visits and hospitalizations, and improved performance on medication-related quality measures common in value-based contracts.
6. Care Transitions Management
The period following hospital discharge represents the highest risk for complications and readmissions—costly events that significantly impact value-based care performance. Comprehensive care management services implement structured transition protocols that bridge the gap between inpatient and outpatient settings.
Care managers ensure timely post-discharge contact, verify medication reconciliation, confirm follow-up appointments, assess for red flags, and provide patient education about warning signs. They also facilitate communication with the patient's primary care team to ensure continuity of the care plan.
Effective transitions management reduces preventable readmissions, improves patient satisfaction, and addresses one of the most significant financial risks in value-based care arrangements where hospitals may face penalties for excess readmissions.
7. Social Determinants of Health Integration
Health outcomes depend substantially on non-medical factors including housing stability, food security, transportation access, and social support. Value-based care models increasingly recognize that addressing social determinants represents a crucial strategy for improving outcomes and controlling costs.
Care management services screen patients for social needs and connect them with appropriate community resources. Care managers develop partnerships with local agencies, create warm handoffs rather than simply providing referrals, and follow up to ensure patients successfully access needed support.
By addressing fundamental needs like nutrition, housing, and transportation, care management services remove barriers to health that no amount of clinical care can overcome. This holistic approach improves patient outcomes improvement while preventing costly acute care utilization driven by unmet social needs.
8. Data Analytics and Performance Monitoring
Value-based care requires continuous monitoring of quality metrics, utilization patterns, and cost trends. Effective care management services incorporate robust analytics capabilities that provide actionable insights to care teams and organizational leaders.
Care managers use data dashboards to track their assigned patient populations, identify gaps in care, monitor progress toward quality benchmarks, and prioritize outreach activities. At the organizational level, analytics reveal performance trends, highlight improvement opportunities, and demonstrate the return on investment from care management activities.
Real-time data integration enables care teams to respond quickly to emerging issues, such as missed appointments, emergency department visits, or abnormal lab results. This responsiveness prevents small problems from becoming costly complications, directly supporting value-based care objectives.
9. Care Team Support and Provider Collaboration
Primary care providers face increasing demands with limited time. Care management services extend the capacity of clinical teams by handling time-intensive activities like patient education, care coordination, barrier identification, and follow-up monitoring.
Care managers serve as the eyes and ears of the provider between visits, maintaining regular patient contact and escalating concerns when clinical intervention is needed. They prepare providers with relevant information before appointments, making clinical encounters more efficient and effective.
This collaborative approach allows physicians to focus on diagnosis and treatment decisions while ensuring patients receive the comprehensive support necessary for successful chronic disease management and preventive care—both essential to value-based care success.
10. Population Health Management at Scale
Value-based care contracts typically hold organizations accountable for entire patient populations rather than individual encounters. Managing population health requires systematic approaches that identify needs, stratify risk, deploy appropriate interventions, and monitor outcomes across thousands of patients.
Comprehensive care management services provide the infrastructure for population health management, including registry functionality, outreach campaigns for preventive services, panel management tools, and workflow systems that ensure no patient falls through the cracks.
Care managers work from prioritized lists that highlight patients needing specific interventions—overdue screenings, uncontrolled chronic conditions, recent hospitalizations, or identified social needs. This systematic approach ensures care teams efficiently address population health needs while maximizing impact on value-based performance measures.
Building the Foundation for Value-Based Success
The transition to value-based care represents both a challenge and an opportunity for healthcare organizations. Success requires moving beyond reactive, episodic care delivery toward proactive, coordinated systems focused on keeping patients healthy and managing chronic conditions effectively.
Comprehensive care management services provide the essential infrastructure for this transformation. By implementing these ten strategies, organizations position themselves to excel in value-based arrangements while delivering better experiences and outcomes for their patients.
The investment in robust care management capabilities pays dividends through improved quality measure performance, reduced acute care utilization, enhanced patient satisfaction, and ultimately, financial success under value-based payment models. As value-based contracts become increasingly prevalent, organizations with mature care management services will maintain competitive advantages and sustainable financial performance.
Healthcare leaders should evaluate their current care management capabilities, identify gaps relative to these ten areas, and develop strategic plans to build comprehensive coordinated care solutions. The future of healthcare reimbursement demands nothing less than a fundamental commitment to managing patient populations proactively, and care management services provide the means to achieve that goal.
Discover how Circle Healthcare's advanced care management platform can help your organization implement these strategies and thrive in value-based care arrangements.

